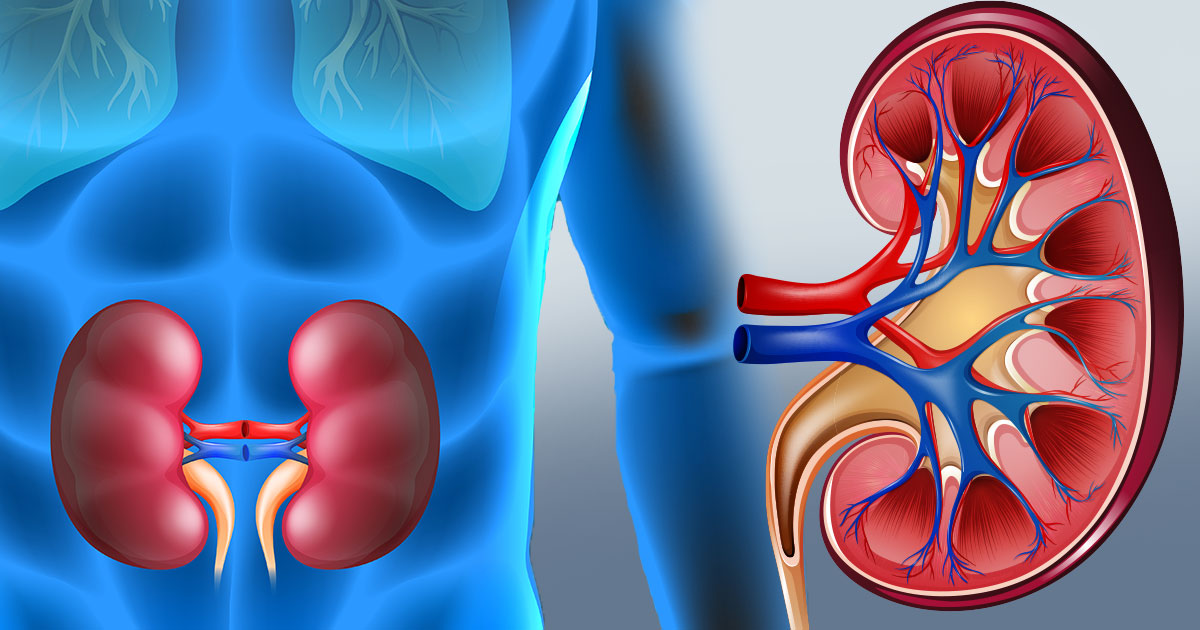
Kidney Disease: Understanding the Basics
Kidney disease refers to conditions that damage the kidneys, which are responsible for filtering blood, producing urine, and regulating fluid and acid levels in the body. When damaged, the kidneys struggle to filter waste, balance fluids, and control blood pressure, which can lead to complications like weak bones, nerve damage, and malnutrition.
As kidney function declines, waste and fluid can build up, causing symptoms such as swelling in the ankles, nausea, weakness, poor sleep, and shortness of breath. If untreated, kidney failure can occur, posing a life-threatening risk.
Types of Kidney Disease
- Chronic Kidney Disease (CKD)
CKD is the gradual loss of kidney function over months or years, often due to changes in kidney structures, such as blood vessels and filtering units (nephrons). As kidneys lose their ability to filter toxins and excess fluid, the condition worsens over time.
- Acute Kidney Disease (Acute Kidney Injury)
Acute kidney injury (AKI), also known as acute renal failure, involves a rapid decline in kidney function within seven days. It can be caused by:
- Prerenal: Decreased blood flow to the kidneys.
- Intrarenal: Direct damage to the kidneys.
- Postrenal: Blockage of urine flow from the kidneys.
Causes
Acute kidney disease causes:
- Not enough blood flow to the kidneys
- Urine backed up in the kidneys
- Direct damage to the kidneys
- Traumatic injury
- Have an enlarged prostate or kidney stones that block urine flow
- Are dehydrated or your muscle tissue breaks down, sending too much kidney toxic protein into your bloodstream.
Chronic kidney disease causes:
- Diabetes (Type 1 and 2)
- High blood pressure
- Heart disease
- Kidney stone
- Obesity
- Family history
- Personal history of acute kidney injury (AKI)
- Smoking
“When damaged, the kidneys struggle to filter waste, balance fluids, and control blood pressure, which can lead to complications like weak bones, nerve damage, and malnutrition.”
Risk factors
AKI risk factors
- A family history of AKI
- Kidney disease
- Heart disease
- Uncontrolled hypertension
- Taking insulin for diabetes
- Liver cirrhosis
- Being over 65
- Being severely dehydrated
CKD risk factors
- A family history of CKD
- High blood pressure
- Heart disease
- Old age
- Diabetes
Symptoms
Warning sign
- Weakness
- Poor appetite
- Dry,scaly skin
- Fatigue
- Trouble sleeping
- muscle cramping
- Dry skin
- Frequent urination,especially at night
- puffiness around the eye
Severe symptoms
- Changes in urine output
- Vomiting
- Nausea
- Fluid retention
- Anemia
- Inflammation of the pericardium
- Hyperkalemia
Diagnosis
- Physical exam
- Ultrasound
- CT scan
- Glomerular filtration rate(GFR)
- Blood creatinine test
- Urine test: albumin
- Kidney biopsy
Treatment and management
Acute kidney disease treatment
Acute kidney injury requires immediate trearment and may be reversible if diagnosed and treated quickly.
- Intravenous (IV) fluids
- Potassium binding drug to remove excess blood potassium
- Calcium gluconate
- Diuretics
- Hemodialysis
Chronic kidney disease treatment
Lifestyle changes
- Limiting salt intake
- Avoid smoke
- Maintaining a healthy weight
- Maintain blood sugar and high blood pressure
- Limiting protein intake
- Healthy diet
- Exercise
Medications
- Diuretics (Loop)
- Iron supplements
- Calcium supplement
- Potassium binder
- stain drugs
- ACE inhibitors
Dialysis
- Hemodialysis
- Peritoneal dialysis
Kidney transplant
A kidney transplant is another treatment option for ESRD.
Prevention
- Drink plenty of water
- Maintain blood sugar
- Maintain high blood pressure
- Reduce salt intake
- Avoid smoke ,alcohol
- Exercise
- Healthy food
- Regular health checkup
Complication
- Hypertension
- Gout
- Heart disease
- Kidney failure
- Anemia
- Metabolic acidosis
- Bone weakness
- Malnutrition