What is Endometriosis?
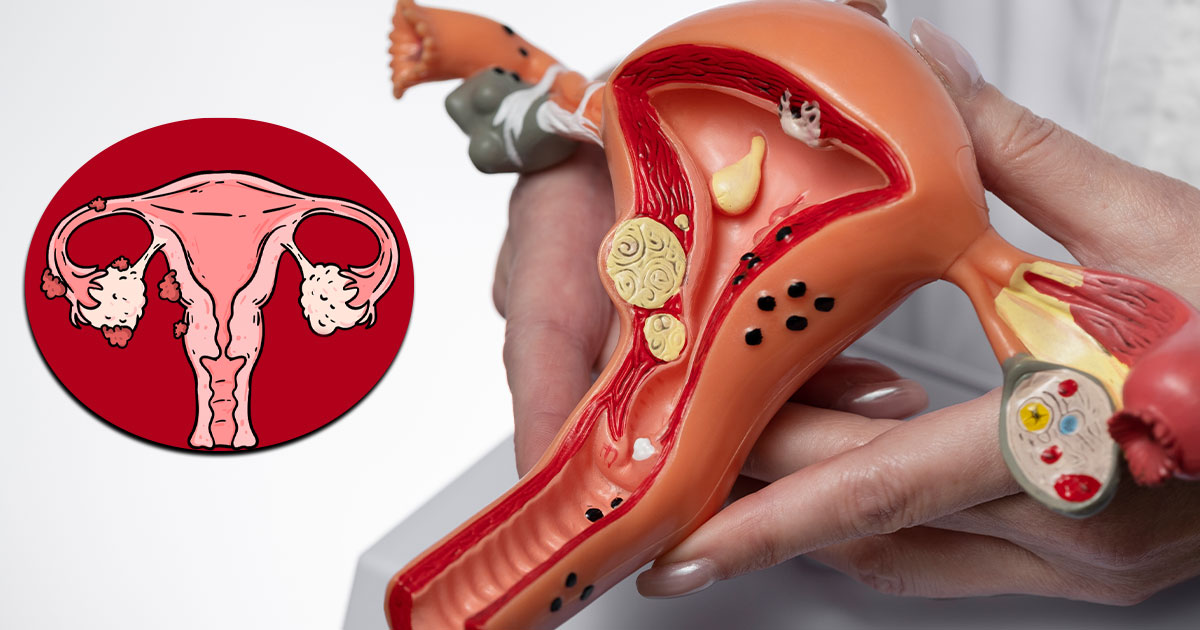
Endometriosis is a condition that primarily affects females. It occurs when tissue similar to the endometrial lining of the uterus grows outside of the uterus. This condition can be difficult to diagnose and carries several complications.
Endometriosis happens when endometrial-like tissue grows on the ovaries, bowel, and the tissues lining the pelvis. Though it is rare for this tissue to spread beyond the pelvic region, it is not impossible. The misplaced tissue, known as endometrial implants, reacts to hormonal changes during the menstrual cycle, becoming inflamed and painful.
This tissue grows, thickens, and breaks down, but unlike normal endometrial tissue, it has nowhere to go. As a result, the tissue gets trapped in the pelvis. While the exact cause of endometriosis is unknown, it is believed to occur when endometrial tissue grows outside the uterine cavity, leading to painful symptoms, often exacerbated by hormone fluctuations.
Types of Endometriosis
Endometriosis can be classified into four main types based on the area it affects in the pelvis or abdomen:
- Endometriomas (Chocolate Cysts): These are dark, fluid-filled cysts, most commonly found on the ovaries.
- Superficial Peritoneal Endometriosis: This is the least severe form, where the endometrial-like tissue is found on the peritoneum (the lining of the abdominal cavity).
- Abdominal Wall Endometriosis: In rare cases, endometrial tissue can grow on the abdominal wall, possibly attaching to surgical scars, such as those from a C-section.
- Deeply Infiltrating Endometriosis (DIE): In this more severe form, the endometrial tissue infiltrates organs within or outside the pelvic cavity, including the ovaries, rectum, bladder, and bowels. This can sometimes lead to the formation of scar tissue that binds organs together.
Causes of Endometriosis
While the exact cause of endometriosis remains unclear, several factors may contribute:
- Genetics
- Surgical procedures (e.g., C-sections)
- Low immune system function
- Hormonal disorders
- Retrograde menstruation (when menstrual blood flows backward into the pelvic cavity)
- Stress
- Obesity
Other potential causes may include:
- Transformation of peritoneal cells
- Surgical scar implantation
- Embryonic cell transformation
- Endometrial cell transport
Risk Factors
Certain factors increase the likelihood of developing endometriosis, including:
- A family history of endometriosis
- A low BMI
- Obesity
- Never having given birth
- High estrogen levels
- Late menopause
- Short menstrual cycles (less than 28 days between periods)
- Early onset of menstruation
- Heavy periods lasting more than a week
Symptoms of Endometriosis
The symptoms of endometriosis can vary, but common signs include:
- Chronic lower back and pelvic pain
- Painful cramping
- Blood in the stool or urine
- Heavy menstrual bleeding
- Periods lasting more than 7 days
- Fatigue
- Nausea and vomiting
- Pain during intercourse
- Urinary and bowel problems (e.g., diarrhea, constipation)
- Spotting or bleeding between periods
- Difficulty getting pregnant
Diseases with Similar Symptoms
Due to the overlap in symptoms, diagnosing endometriosis can be difficult. Conditions with similar symptoms include:
- Ovarian cysts
- Irritable bowel syndrome (IBS)
- Pelvic inflammatory disease (PID)
Diagnosis
A proper diagnosis of endometriosis may require several tests, including:
- Medical history review
- Blood tests
- Pelvic exam
- Ultrasound
- MRI
- Transvaginal ultrasound
- Laparoscopy
- Biopsy
Treatment for Endometriosis
While there is no cure for endometriosis, treatment typically involves a combination of medication and surgery. Finding the right treatment often requires trial and error.
- Pain relief: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help alleviate pain.
- Hormone therapy: Supplemental hormones can relieve pain and slow the progression of endometriosis. Hormonal therapies regulate the menstrual cycle, reducing tissue growth.
- Hormonal contraceptives: Birth control pills, patches, or vaginal rings can help reduce or eliminate pain.
- Danazol (Danocrine)
- Progestin-only contraceptives
- Gonadotropin-releasing hormone (GnRH) agonists and antagonists, such as elagolix sodium (Orilissa) or leuprolide (Lupron)
Surgical Options:
- Conservative surgery: Laparoscopy can remove or destroy the endometrial tissue.
- Last resort surgery: A hysterectomy may be considered in severe cases.
Stages of Endometriosis
Endometriosis is classified into four stages based on severity:
- Stage 1 (Minimal): Small lesions or shallow implants on the ovaries and pelvic cavity with mild inflammation.
- Stage 2 (Mild): Light lesions and shallow implants on the ovaries and pelvic lining.
- Stage 3 (Moderate): Deep implants on the ovaries and pelvic lining, with numerous lesions.
- Stage 4 (Severe): Extensive deep implants on the pelvic lining and ovaries, with lesions on the fallopian tubes and bowels.
Prevention
While endometriosis cannot be fully prevented, certain lifestyle changes may help manage symptoms:
- Maintain a healthy diet and weight
- Exercise regularly
- Be aware of early symptoms
- Use hormonal birth control
- Avoid caffeine, smoking, and excessive alcohol consumption
- Maintain personal hygiene
Complications
Endometriosis can lead to several complications, including:
- Heavy bleeding during or between periods
- Depression and anxiety
- Infertility
- Chronic pelvic pain
- Chest pain or shortness of breath (in severe cases)
- Ectopic pregnancy
- Ruptured cysts
- Bladder and bowel problems
- Nausea and fatigue