Nepalese medical professionals have initiated prominent demonstrations to express concerns about major issues affecting both their professional lives and personal well-being.
Postgraduate stipends and bonds in private medical colleges, alongside workplace safety, regulated working hours, and labor exploitation, have become the focus of these protests.
The demonstrations have sparked conversations across the country about the healthcare system, the rights of workers in essential professions, and their treatment.
The Stipend and Bond Controversy
Postgraduate medical students, particularly those in private institutions, have long felt marginalized due to disparities in stipends and the imposition of mandatory service bonds.
While their counterparts in government colleges receive standardized allowances, many residents in private colleges either receive significantly less or no stipend at all. For students who have already spent millions of Nepali rupees on their education, this lack of financial support is a crushing burden.
Addressing stipend, working hours, and bond disparities requires joint efforts from the Government of Nepal, private medical institutions, and key stakeholders to ensure fair pay, workload balance, and the removal of financial limitations to postgraduate education.
Moreover, the issue of mandatory service bonds adds to the frustration. Many postgraduate students are required to sign contracts obligating them to work in specific locations or institutions after graduation.
While the intention behind this policy is to address the shortage of medical professionals in underserved areas, it often ends up being exploitative.
Doctors are frequently placed in resource-scarce environments with minimal support, making it difficult for them to provide quality care while coping with their own professional development.
In response, the ‘Safe Workplace for Health Worker Struggle Committee’ has been vocal in rejecting recent agreements between government ministers, labeling them as dishonorable to Nepali doctors.
Their demands are clear: align the allowances for resident doctors in private institutions with government standards and eliminate fees and bonds associated with postgraduate programs.
This appeal for equity corresponds with the overall drive for fair treatment in the medical profession.
The gravity of the situation intensified when resident doctors threatened to discontinue non-emergency treatments if their concerns were not addressed immediately.
Such a decision demonstrates the depth of their dissatisfaction with the Nepal Medical Association, Medical Education Commission, and Government of Nepal, as well as the possible impact on Nepal’s healthcare system, which heavily depends on these specialists.
The Quest for Safe Workplaces
Aside from financial issues, doctors are also concerned about increased workplace violence.
Physical assault, verbal abuse, and threats from patients or families are all too common in Nepal’s healthcare institutions.
Several qualitative studies have indicated that physical violence against healthcare professionals by patients or their relatives can be complex and multifaceted.
Patients often express frustration when outcomes surpass their expectations, and a lack of robust institutional protections exacerbates the matter.
These stressful circumstances not only impair doctors’ mental health but also compromise the care they deliver to patients.
Many doctors have reported working in a constant state of fear and anxiety. This issue is further aggravated by a lack of proper security measures in hospitals.
Security personnel are often either absent or ill-equipped to handle volatile situations, leaving doctors vulnerable to harm.
To combat this, doctors have advocated for specific guidelines for reporting incidents, severe punishments for perpetrators, and mental health support for those affected by violence.
A safe workplace is more than just a demand; it is necessary to ensure that doctors can focus on their jobs without fear of bodily or mental injury.
Regulating Working Hours and Addressing Labor Exploitation
Many doctors in Nepal are forced to work long, unrestricted hours, which causes physical and emotional exhaustion.
Junior doctors, particularly residents and interns, are sometimes posted to work shifts that last more than 48 hours, with few or no breaks.
Such practices jeopardize not just the doctors’ well-being but also the safety of patients because exhausted and unmotivated doctors are more likely to make critical errors.
The broader issue of labor exploitation extends to mandatory bonding service programs.
These programs, while intended to address healthcare inequities, often lack fairness and proper implementation.
Doctors in these programs frequently report being overworked and under-resourced, with little acknowledgment of the personal sacrifices they make.
Moreover, medical graduates working under these bonds are often paid salaries that are far below market standards.
This creates a system where young doctors feel trapped—unable to refuse the bond due to contractual obligations, yet dissatisfied with the conditions they are forced to endure.
A study examining the experiences of medical graduates under such bonding programs revealed significant challenges, including inadequate support and resources, leading to feelings of exploitation and dissatisfaction.
Broader Implications for Nepal’s Healthcare System
The protests highlight systemic issues within Nepal’s healthcare system that go beyond the immediate grievances of doctors.
Due to a lack of proper attention and insufficient investment by the Government of Nepal in public healthcare infrastructure, private medical colleges and institutions have taken substantial control of the medical education and health system.
The profit-driven nature of many private medical institutions and hospitals often results in prioritizing financial gain over student and staff well-being.
Doctors are not protesting only for better working conditions for themselves but also for a fair and sustainable national healthcare system.
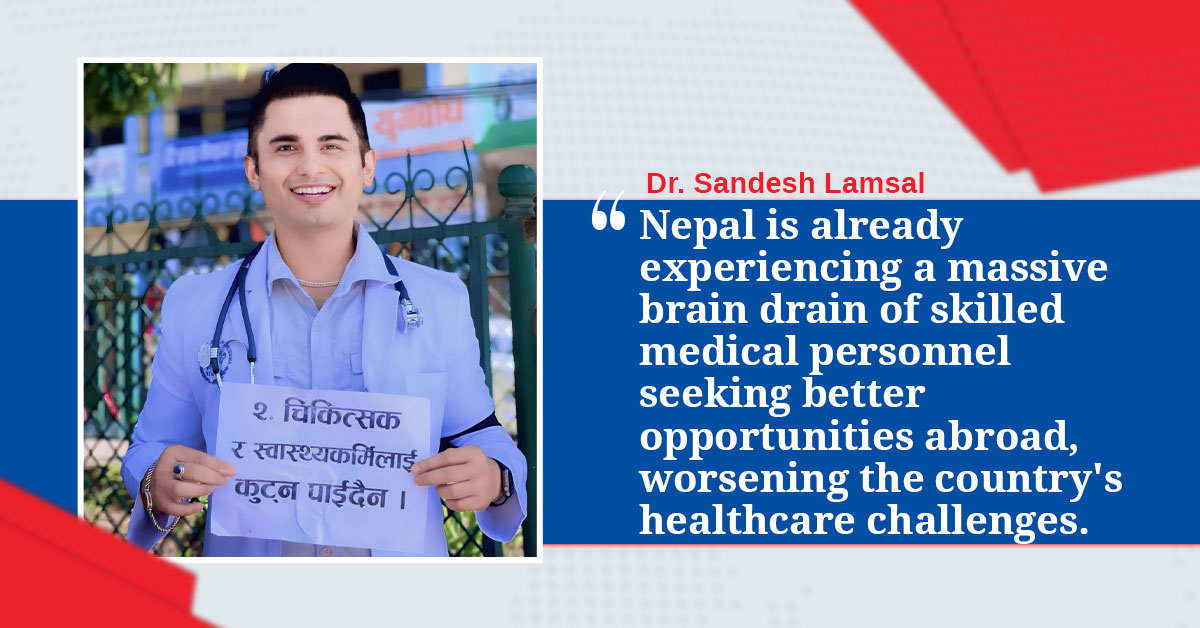
Nepal is already experiencing a massive brain drain of skilled medical personnel seeking better opportunities abroad, worsening the country’s healthcare challenges.
Ignoring the demands of the ongoing doctors’ protests could catastrophically impact Nepal’s healthcare system.
A Call for Comprehensive Reform
The collective grievances of Nepal’s medical community point to a pressing need for comprehensive reform.
Providing adequate support, resources, and incentives can make service in underserved areas more appealing without resorting to coercive measures.
Addressing stipend, working hours, and bond disparities requires joint efforts from the Government of Nepal, private medical institutions, and key stakeholders to ensure fair pay, workload balance, and the removal of financial limitations to postgraduate education.
Ensuring safe workplaces requires the implementation of strict regulations that protect healthcare professionals from violence, harassment, discrimination, and work overload.
This involves creating clear standards for reporting events, providing support networks for victims, conducting proper and unbiased investigations, and imposing strict consequences on perpetrators.
Implementing standardized working hours, guaranteeing adequate rest, decent salaries, incentives, promotions, and encouraging a good work-life balance is critical for preventing burnout and ensuring the well-being of doctors, residents, and interns.
Lastly, addressing labor exploitation involves re-evaluating mandatory bonding programs to ensure they serve their intended purpose without infringing on the rights and freedoms of doctors.
Providing adequate support, resources, and incentives can make service in underserved areas more appealing without resorting to coercive measures.