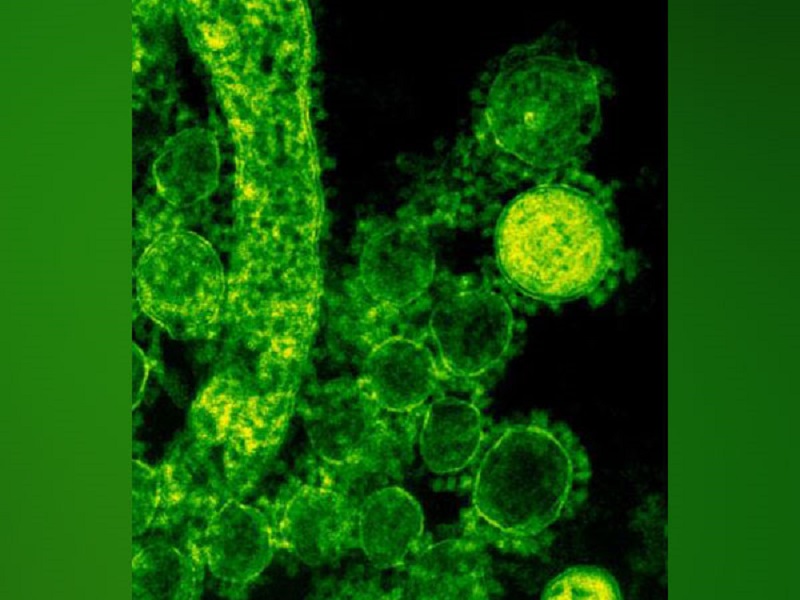
The yeast Candida is the most infamous of all the fungi that inhabit the human body. This distant relative of baker’s yeast is well known for producing several different varieties of thrush, which can be quite bothersome, but it can also result in an invasive infection, which can occasionally be fatal.
A research team from the Weizmann Institute of Science led by Prof. Jakub Abramson discovered a previously unidentified immune system defensive mechanism used to combat Candida infections in the study.
This study was published in the journal Nature Immunology.
Most healthy individuals have low levels of candida in their bodies, which is a component of the microbiome, a diverse range of microbes that live in harmony on our skin and in our gut. Candida is normally kept in check by the immune system, but on rare occasions, it can grow out of control and invade the skin, vaginal lining, mouth lining, or other parts of the body. It may become severe enough to spread to the bloodstream, where it may then reach the kidneys. These potentially fatal infections can arise when an individual’s immune system has been compromised, for instance by AIDS or by immunosuppressive medications like cancer chemotherapy or steroids.
By giving this yeast an unfair advantage over other microorganisms, antibiotics, which eradicate many of the beneficial bacteria in our microbiome, can also cause local or invasive Candida eruptions. This explains why women occasionally get a vaginal yeast infection after taking antibiotics, for example.
The small, globular lymphocytes of the T cell type, known as TH17, were previously credited with protecting the body against Candida. When this defense fell short, it was these cells who bore the brunt of the blame.
In the new study, postdoctoral fellow Dr. Jan Dobe and colleagues in the Abramson lab at the Weizmann Institute of Science’s Department of Immunology and Regenerative Biology found that a commando unit of TH17 cells capable of fighting Candida cannot be produced without critical early support from an entirely different contingent: a subset of uncommon lymphoid cells known as type-3 innate lymphoid cells, or ILC3, that express a gene known as the autoimmune regulator, or A.
The two cell groups are a part of the immune system’s two distinct arms, which work together against a common foe like specialized units and foot patrols. The Aire-ILC3s, which are a component of the more primitive, innate arm, react almost instantly to a threat, in this case, a Candida infection.
The TH17s is a part of the more recent adaptive arm of the immune system, which takes several days or even weeks to react but launches a much more focused and effective attack than the innate one.
The researchers discovered that the Aire-ILC3s swallow the yeast whole, break it up, and display some of the pieces on their surfaces as soon as Candida begins to infect tissues. The TH17s, some of which are typically on call in the lymph nodes and prepared for an infection alert, are given these bits in that manner. The sspecializedT cells are given instructions to divide quickly, increasing their population from a few lone commandos to hundreds or even thousands of Candida-specific fighters that can eradicate the yeast at the infection sites.
According to Abramson, “We have discovered a previously unknown immune system weapon that is essential for coordinating an efficient response against the fungal infection.”
Because Candida frequently causes severe, ongoing infections in people with a rare autoimmune syndrome brought on by defects in the Aire gene, Abramson became fascinated by the condition. This gene had been the subject of extensive research in Abramson’s lab, which helped to define its function in preventing autoimmune diseases. That study, along with research by other scientists, demonstrated that Aire-expressing cells in the thymus give developing T cells instructions not to attack the body’s own tissues. When Aire is damaged, T cells do not receive the correct instructions, which leads to widespread autoimmunity that causes damage to numerous body organs. But there was still a mystery: Why would patients with aire deficiency who were also suffering from severe autoimmune syndromes get chronic Candida infections?
In an effort to solve the Aire puzzle, Dobe and colleagues discovered that a small subset of ILC3s in the lymph nodes also express Aire outside of the thymus. The scientists next genetically modified two groups of mice: one group was deficient in Aire in the thymus and the other in the ILC3s in the lymph nodes. The initial group experienced autoimmunity but was able to defeat Candida. The second group, those lacking Aire in ILC3s, did not have autoimmunity in contrast, but they were unable to produce a lot of Candida-specific TH17s. As a result, they were unable to successfully eradicate Candida infections. To put it another way, the number of specialized cells required to combat Candida was not produced in the presence of Aire-expressing ILC3s.
Dobe says, “We discovered an entirely new function for Aire, one that it plays in the lymph nodes — activating a mechanism that boosts the quantity of Candida-fighting T cells.
These findings open up new research avenues that could eventually lead to the development of new medications for severe Candida infections as well as perhaps other fungal infections. The recently discovered mechanism, for instance, could aid in the production of numerous Candida-fighting T cells for cell therapy. And if researchers ever discover the signals that Aire-ILC3s use to stimulate T cell proliferation, those signals themselves might serve as the foundation for fresh treatments.